Detailed Overview for Healthcare Professionals
The regulation of thyroid hormones is governed by the hypothalamic-pituitary-thyroid (HPT) axis, a key system for maintaining metabolic equilibrium across all major body systems. The hormones Thyroxine (T4) and Triiodothyronine (T3), synthesized and released by the thyroid, play essential roles in cellular function and energy metabolism. A deficiency of these hormones, as seen in hypothyroidism, slows down metabolic processes, leading to significant physiological and clinical consequences.
Hormonal Regulation Process in the HPT Axis
- Initiation at the Hypothalamus and TSH Release
The regulation process begins in the hypothalamus, which, in response to signals about the body’s metabolic needs, releases thyrotropin-releasing hormone (TRH). TRH travels to the anterior pituitary gland, prompting it to release Thyroid Stimulating Hormone (TSH) into the bloodstream. This TSH is a critical activator for the thyroid gland, where it binds to specific receptors and stimulates the production of T4 and T3. - Production of T4 and Peripheral Conversion to T3
Within the thyroid gland, the primary product is T4, which is released into the bloodstream. T4 is considered a prohormone and is converted in peripheral tissues to the active hormone T3 by the enzyme deiodinase. The liver, kidneys, and muscles play major roles in this conversion. T3, the biologically active form, binds to nuclear receptors in cells throughout the body, regulating gene expression and thereby controlling processes like energy production, lipid metabolism, and thermogenesis. - Negative Feedback Mechanism and Metabolic Control
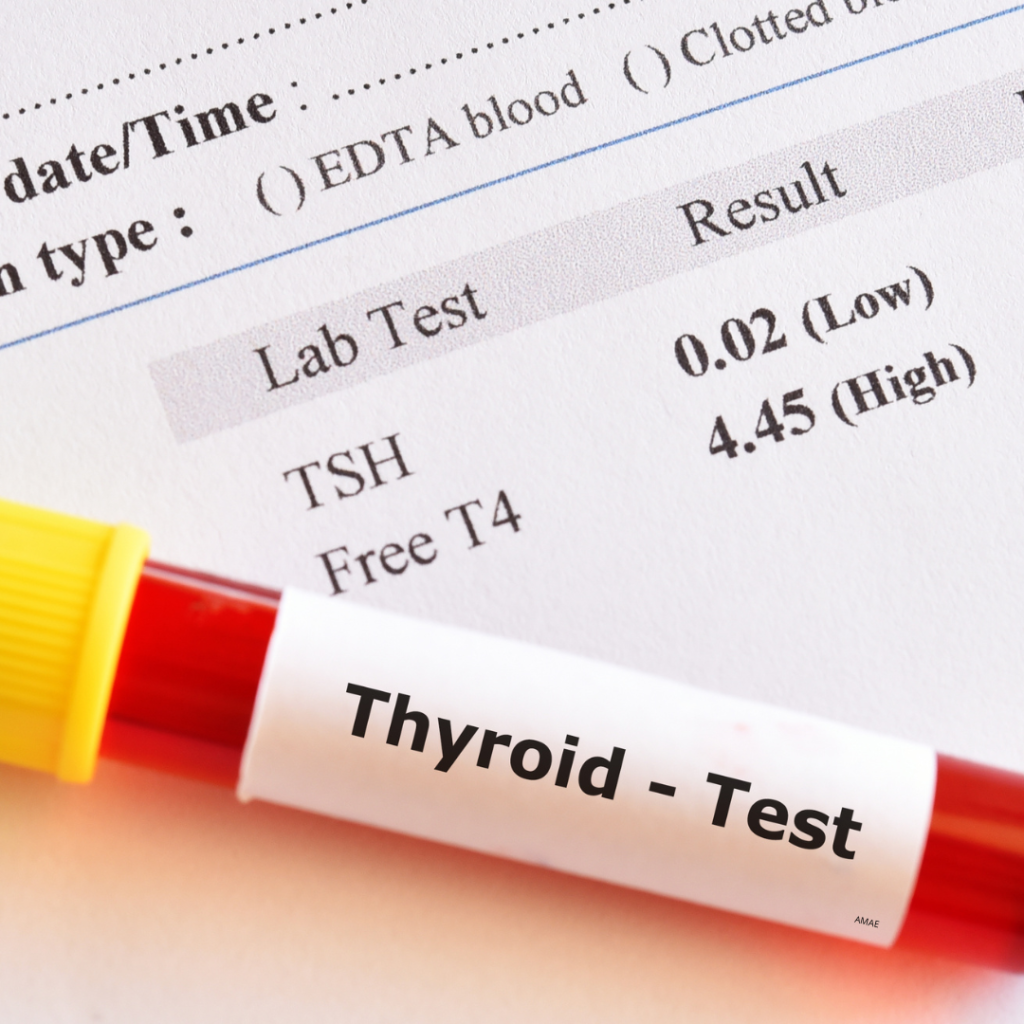
The negative feedback loop within the HPT axis is essential for maintaining appropriate thyroid hormone levels. Low levels of circulating T4 and T3 stimulate TSH release, increasing thyroid hormone synthesis, while elevated T4 and T3 levels suppress TSH secretion, reducing hormone production. In primary hypothyroidism, where the thyroid fails to produce adequate T4 and T3, TSH levels remain persistently high as the body attempts to stimulate thyroid function, but low levels of T4 persist. This results in elevated TSH and low T4, hallmark indicators of hypothyroidism in lab testing.
Clinical Significance in Diagnosing Hypothyroidism
- Interpretation of Thyroid Hormone Levels
In primary hypothyroidism, the classic laboratory profile includes elevated TSH with low free T4 levels, clearly indicating thyroid dysfunction. In subclinical hypothyroidism, TSH is mildly elevated while T4 and T3 levels remain within normal ranges. This scenario often reflects an early stage of thyroid dysfunction and requires consideration of factors such as age, symptomatology, and cardiovascular risk when determining treatment necessity. Subclinical hypothyroidism, while generally asymptomatic, can progress to overt hypothyroidism, especially in patients with positive thyroid antibodies or specific risk factors. - Factors Affecting Diagnosis and Management
Accurate diagnosis relies on thorough lab work and clinical evaluation. TSH levels should be measured in patients presenting with symptoms such as fatigue, weight gain, cold intolerance, and constipation. However, factors like non-thyroidal illness, certain medications, and pregnancy can influence TSH and T4 levels, potentially complicating diagnosis. A comprehensive review of the patient’s medication history and concurrent conditions is crucial for accurate interpretation.
Treatment Implications and the Importance of the HPT Axis in Therapy
- Guiding Thyroid Hormone Replacement Therapy
An understanding of HPT axis dynamics is vital for effectively administering and adjusting T4 replacement therapy. TSH levels serve as the primary guide for adjusting levothyroxine dosage to ensure the patient’s T4 levels are optimized. Over-replacement can lead to adverse outcomes such as tachycardia, unintentional weight loss, and insomnia, especially in elderly patients or those with cardiovascular conditions. Dose adjustments must be gradual, with follow-up testing every 6-8 weeks until TSH stabilizes within the desired range. - Challenges in Treatment and Monitoring
Monitoring TSH levels regularly is essential in managing hypothyroid patients, especially after initial diagnosis or following dose adjustments. Patients should be advised to take their T4 medication consistently, preferably in the morning on an empty stomach, to enhance absorption. Annual TSH checks are recommended for stable patients; however, increased frequency may be warranted in cases of pregnancy, medication changes, or symptom fluctuations. - Special Populations and Considerations
Special populations, including pregnant women and elderly patients, may require individualized treatment strategies. During pregnancy, thyroid hormone demands increase, and hypothyroid patients often need a 20-50% dose increase. Close monitoring of TSH and T4 levels is crucial throughout gestation to prevent adverse outcomes. In elderly patients, sensitivity to thyroid hormones is higher, making conservative dosing and gradual adjustments critical to avoid complications.
References
- Surks, M. I., Ortiz, E., Daniels, G. H., et al. (2004). Subclinical thyroid disease: scientific review and guidelines for diagnosis and management. JAMA, 291:228–238.
- Rodondi, N., den Elzen, W., Bauer, D., et al. (2010). Subclinical hypothyroidism and the risk of coronary heart disease and mortality. JAMA, 304(12):1365–1374.
- Weetman, A. P., Jameson, J. L. (2005). Disorders of the thyroid gland. In: Kasper, D. L., Braunwald, E., Fauci, A. S., et al., eds. Harrison’s Principles of Internal Medicine. 16th ed. New York: McGraw-Hill, Chapter 220, Part 14, Section 1.
- Garber, J. R., Cobin, R. H., Gharib, H., et al. (2012). Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Endocr Pract., 18(6):988-1028.
- Jonklass, J., Bianco, A. C., Bauer, A. J., et al. (2014). Guidelines for the treatment of hypothyroidism: prepared by the American Thyroid Association Task Force on thyroid hormone replacement. Thyroid, 24(12):1670–1751.
- Pizzorno, L., Ferril, W. (2006). Thyroid. In: Jones, D. S., ed. Textbook of Functional Medicine. Gig Harbor, WA: The Institute for Functional Medicine, pp. 644–650.
- Ruchała, M., Szczepanek-Parulska, E., Zybek, A. (2012). The influence of lactose intolerance and other gastro-intestinal tract disorders on L-thyroxine absorption. Endokrynol Pol, 63(4):318–323.
- Rose, S. R. (2010). Improved diagnosis of mild hypothyroidism using time-of-day normal ranges for thyrotropin. J Pediatrics, 157(4):662–667.
- Siegmund, W., Spieker, K., Weike, I., et al. (2004). Replacement therapy with levothyroxine plus triiodothyronine (bioavailable molar ratio 14:1) is not superior to thyroxine alone to improve well-being and cognitive performance in hypothyroidism. Clin Endocrinol, 60:750–757.
- Vanderpump, M. P. J. (2010). How should we manage patients with mildly increased serum thyrotrophin concentrations? Clin Endocrinol, 72:436–440.